Case Study in Prepatellar Bursitis
Case Study in Prepatellar Bursitis
By: Julia Trimble
Introduction:
Surrounding large synovial joints are small fluid-filled sacs composed of fibrous connective tissue called Bursa Sacs. They are found in any area that ligaments and tendons articulate with bones or skin.[1] Some Bursae are superficial and they separate bone from the subcutaneous layer of the skin while thers lay behind or within synovial joints. Bursae are lined with synovial tissue containing a viscious, nutrient-rich liquid called synovial fluid.1 This fluid acts as a slippery cushion that keeps surfaces from rubbing against each other but also to absorb extra pressure on the joints.
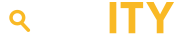
In the knee, there are only five major bursae surrounding the patella.[1] Two of the bursae located near one another are the superficial and deep infrapatellar bursae. The superficial infrapatellar bursa is located inferior to the patella and separates the patellar tendon from skin. The deep infraptellar bursa, although is also located inferior to the patella, is behind the tendon. It separates the Tibia from the patellar tendon. Another bursa is the Suprapatellar bursa and it is located superior to the patella and separates the femur from the quadriceps femoris. The pretibial bursa is located inferior to the patella and it superficially separates the tibia from the skin at the tibial tuberosity.2 Finally, the prepatellar bursa lies superficial to the patella and separates the patellar bone from the integument.2 As a group, all bursae function to disperse force and pressure on the knee joint and act as shock absorbers for the femoral and tibial bones. They also reduce friction during the articulation of the patella, tibia, and femur.[2] The prepatellar bursa is especially helpful in reducing friction between bone and skin when pressure is applied to the knee very often. When stress occurs in this area too often, complications can occur.
Explanation:
Prepatellar bursitis is a disease that occurs when the bursa sac located anterior to the knee becomes damaged due to either a trauma or infection that causes an inflammatory response.3 In most situations, the body’s purpose for inflammation is to isolate or immobilize a damaged region of the body to either avoid further injury or the possible spread of infection.
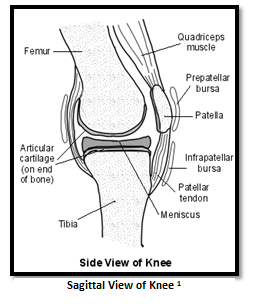
Prepatellar Bursitis appears in two forms: septic or aseptic. Each varies depending on its cause. Septic bursitis is the inflammation of bursa as a result of an infection. The infection usually occurs when the microbe Staphylococcus Aureus enters the body through a cut in the skin (most often around the knee). [3] The other form of prepatellar bursitis is the aseptic form that is caused by continuous stress or acute trauma to the knee. Damage to this area causes the bursa to swell up, thus limiting the range of motion to the joint. It is vitally important to distinguish the difference between septic and aseptic bursitis so as to administer the correct form of treatment. In order to determine the difference, a sample of the synovial fluid can be extracted or “aspirated” from the bursa and cultured in a sterile environment if septic bursitis is suspected.4 During the culture, certain indications of an infection may include heightened levels of protein, lactate, or a white cell count. There may also be a lowered glucose level and the presence of a gram-negative bacterium (Staphylococcus Aureus).4 To determine aseptic prepatellar bursitis, physicians can perform a physical examination or take MRIs and X-Rays of the knee to look for a distended prepatellar bursa. In most cases, just the physical examination provides enough justification to diagnose chronic prepatellar bursitis, however if the physician isn’t certain, further investigation may be necessary.
Although bursitis is best confirmed via procedural examination, the initial diagnosis is made by the presentation of a series of consistent symptoms and a history of trauma or injury to the knee. A common cause of bursitis is prolonged stress on the knee throughout a long period of time. Prepatellar Bursitis is often called the “housemaid’s knee” because it appears most in individuals that work on their knees, like maids, plumbers, and roofers.4 When the bursa is stressed, the thin tissue around the bursa begins to thicken to compensate for the added pressure. When stressed too much, the bursa becomes inflamed and elevates to prepatellar bursitis. Another cause of bursitis is damage to the bursa sac through trauma. If a patient has had a recent fall or blow to the knee, they may have damaged some of the blood vessels located near the prepatellar bursa. When this happens, blood can flood the sac causing it to swell up and become inflamed.[1] Although the outward appearance may seem minor to the individual, the damage to the actual bursa can be damaging if not treated. This can become a problem when patients downplay their symptoms because of what appears as a simple bruise. In the septic form of bursitis, an infection causes the small amount of synovial fluid within the sac to be replaced with pus from the dead cells that are fighting off the ongoing infection. Patients suffering from prepatellar bursitis may experience reoccurring knee pain followed by possible redness and swelling.5 They may also have difficulty with their range of motion in certain actions like walking, crawling, or kneeling.5 With septic bursitis, redness will be especially apparent and a fever may even occur if the infection is bad enough. Patients with a lowered immune system may require immediate confirmation of diagnosis if they do not present the symptoms of an immune response.
The best way to begin diagnosing prepatellar bursitis is to start with a physical examination. In doing so, you may find tenderness or inflammation above the knee. When asked, the patient may also claim to notice a limited range of movement in the knee joint and pain during articulation.[2] This is dependent on the amount of activity in the patient’s occupation or daily life. The more stress that is put on the bursa, the more inflamed it will become. Another very obvious visual indication of prepatellar bursitis includes a small or large bump above the patella. This bump is the expanded bursa sac filled with excess fluid, blood, or pus depending on the type of bursitis. In the instance of septic bursitis, you may notice redness and warmth on the skin. Some patients may have healed over the cut in the skin that the infection originated from and developed a very painful abscess.6 In some more serious cases of infection, the patient may also present with symptoms of systemic problems, such as a fever or if serious enough, even tachycardia. In which case, this can be a cause for alarm and the patient would then need emergency care.
Most patients are not greatly affected by their prepatellar bursitis. As an aseptic inflammatory response, most people experience slight difficulty in movement and swelling that is no different than any normal injury. The swollen bursa can cause minor pain in some patients while in others it causes no pain at all. The amount of irritation affects people differently depending on their activity levels.6 For employees that develop bursitis through prolonged stress but have no way around occupational obligations will have greater difficulty functioning because the more they work, the worse their condition will get. Without isolation, the patient can cause further injury to the bursa and risk lowering their ability to articulate that joint. Patients with acute trauma usually experience an easy recovery and their condition will not greatly affect their life. If they are able to treat the area as a normal injury, then the body will reabsorb the excess blood over time.6 This is similar to the process of fading an old bruise. Patients with a poor immune system that have septic bursitis run a greater risk of systemic problems if their body is unable to fight off the infection. If spread, the infection can lead to serious, sometimes life-threatening, complications.
Evaluation:
To treat prepatellar bursitis, there are two forms of action: Surgical and Nonsurgical. These treatments can range between medication, therapy, and excision. In minor aseptic cases, prepatellar bursitis can be fixed with bed rest, ice, and compression wraps.[3] For patients who have no choice but to continue stressing the bursa, physicians often suggest knee pads or cushions to relieve stress on the joint during activity along with non-steroid inflammatory pain-relievers like ibuprofen and motrin.6 After doing so, physicians may also refer patients to a physical or occupational therapist to reduce any loss in their range of motion in the knee by increasing the flexibility of their surrounding muscles. If persistent inflammation occurs, physicians may also administer anti-inflammatory steroids such as Hydrocortisone that restricts blood flow through the capillaries and Corticosteroids that affects the body’s immune response to infection.[4] Such infections are first treated with an antibiotic medication like penicillin. In chronic cases, however, antibiotics must be administered through an IV if the patient experiences systemic or immune problems.7
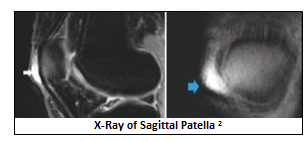
The other form of treatment, surgical, is usually administered after all non-surgical treatments have failed. These steps are taken as a last resort for patients who continue to experience complications with their condition. Some patients experiencing prolonged inflammation from an infection can have the bursa drained by making an incision in the skin above the patella and inserting a tube into the prepatellar bursa and allowing the pus to drain out of the sac for multiple days so that the antibiotics can take effect. Physicians can even insert a large syringe into the bursa sac to extract the fluid to relieve the extra pressure of the swollen bursa. This can only occur if an infection is ruled out. If all else fails and the patient is not cured by any other treatment, they can have a Bursectomy performed to remove the prepatellar bursa altogether. Although surgery always presents risk, this procedure actually has a very good outcome. During a Bursectomy, a surgeon makes an incision above the patella and cuts out the thickened bursa sac. Because the prepatellar bursa lies superficial to the patellar tendon, the surgeon doesn’t cause any muscle damage. After surgery, patients will be expected to rest, staying off of the affect knee, and eventually go to physical therapy to strengthen the surrounding muscles. Over time, the bursa sac often grows back in response to the body’s need to reduce friction between bone and skin. The new bursa often returns the quality of life to the way it was before bursitis.
Of course every treatment has its risks but nearly all procedures for bursitis have good outcomes. In nonsurgical treatments, you run the risk of worsening the condition by not taking further action. Through steroid injections, you can spread further infection if not noticed and there are always risk factors in surgery between anesthesia and sepsis however, the chances of any risks causing lifelong issues to the individual are very slim. This gives the pathology a good prognosis for most patients.
Conclusion:
Prepatellar Bursitis can affect people of all ages but it often appears in young kids and patients with immune system problems. All treatments should be administered based on cause and activity of the patient. For example, an elderly woman in a nursing home would not receive a Bursectomy because with age, it would take longer to heal and lead to more risks to go into surgery. She would most likely receive antibiotics and rest. Workers that consistently put stress their knees should first try knee braces and cushions but as a last resort, may find continual aspirations necessary to relieve the pressure on their knees. If inflammation persists, they may benefit from a Bursectomy, however this would be based upon the patient’s ability to make time for recovery and post-surgical rehabilitation. Other patients, such as the young and immunocompromised have a greater difficulty fighting off the infection involved with prepatellar bursitis. With these patients, an aggressive treatment of antibiotics may be necessary along with a possible immediate drainage of the bursa to allow the antibiotics to take affect before the infection spreads and becomes a problem to their overall health.
Works Cited
Medical Multimedia Group, L.L.C. (n.d.). A Patient’s Guide to Prepatellar Bursitis. Retrieved from Houston Methodist Orthopedics and Sports Medicine: http://www.methodistorthopedics.com/prepatellar-bursitis
Chatra, P. S. (2012). Bursae around the knee joints. Indian Journal of Radiology and Imaging, 22(1), 27-30. Retrieved from http://www.ijri.org/article.asp?issn=0971-3026;year=2012;volume=22;issue=1;spage=27;epage=30;aulast=Chatra
Dr Michelle Wright, D. C. (2013, September 09). Prepatellar Bursitis. (D. J. Cox, Ed.) Retrieved from Patient.co.uk: http://www.patient.co.uk/doctor/prepatellar-bursitis
Kelly L Allen, M. (2012, August 29). Prepatellar Bursitis Treatment and Management. (M. Consuelo T Lorenzo, Editor) Retrieved from Medscape: http://emedicine.medscape.com/article/309014-treatment#a1138
Rodrigo O. Aguiar, F. C. (2007). The Prepatellar Bursa: Cadaveric Investigation of Regional Anatomy with MRI After Sonographically Guided Bursography. American Journal of Roentgenology, 188(4). Retrieved from http://www.ajronline.org/doi/full/10.2214/AJR.05.1466