An Exploration of Antibiotic Sensitivity & Resistance
An Exploration of Antibiotic Sensitivity & Resistance
By: Tyler Ryan
I. Introduction
Understanding antibiotics is crucial to the world of medicine and biology. Antibiotics are a type of medicine used to target and kill bacterial cell infections. A growing issue of concern is that bacteria cells are becoming resistant, or unaffected, by current antibiotics. This makes bacterial infections a much more serious issue. Research has shown that overusing antibiotics is the primary cause for antibiotic resistance (Solomon Berg and Martin 2011, 534). Due to their ability to mutate and reproduce quickly, bacteria cells that are able to survive antibiotics pass on the genetic material to spread the infection. Now, the majority of the population of the bacterial cells are resistant to the antibiotic and the infection is difficult to treat. A closer look at the chemistry of a bacteria cell can give us more information on how to treat them with antibiotics.
We now know that bacteria cells have two types of cell walls: Gram-positive and Gram-negative. Gram-positive cells have a thick peptidoglycan layer that covers the plasma membrane. Gram-negative cells have a thinner peptidoglycan layer than the Gram-positive cells, but the peptidoglycan layer is coated by a layer of polysaccharides with lipoproteins. Understanding this information has allowed the pharmaceutical researchers to distinguish two types of antibiotics. Narrow antibiotics target the peptidoglycan layer of the bacteria cell while broad antibiotics target DNA and RNA. Narrow antibiotics can target either Gram-positive or Gram-negative bacterium. With this, it is understood that narrow antibiotics may be weaker in killing strength but can target specific cells, while broad antibiotics are more powerful yet may kill the wrong bacterial or cause resistance to develop (qtd. in Pinou). One issue that arises is dealing with Gram-negative bacteria. Since their peptidoglycan layer is buried beneath a thicker polysaccharide layer, they are extremely difficult to be targeted by narrow antibiotics. To put this issue into perspective, studies from European hospitals have concluded that out of the near 25,000 annual deaths that occurred from hospital-acquired bacterial infections, it is estimated that about two-thirds of those deaths were Gram-negative bacteria related (Pollack).
The lab experiment was performed from the mindset of a physician. The problem was to determine what antibiotic is best to prescribe to the patient. It can be hypothesized that broad antibiotics will have “killing zones” with larger diameters than the narrow antibiotics will. This is because broad antibiotics can potentially damage other bacteria due to it targeting DNA over the peptidoglycan layer of the bacteria. Also, narrow, Gram-positive antibiotics will have larger killing zone diameters than narrow, Gram-negative antibiotics. The larger the killing zone diameter, the more effective at killing bacteria the antibiotic is. Gram-positive antibiotics will show larger killing zones because Gram-positive bacteria have an easier to target peptidoglycan layer than Gram-negative bacteria because it is not buried by a lipoprotein outer membrane.
II. Materials & Methods
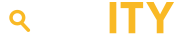
The procedure that was followed for this experiment was similar to the techniques a lab technician and a physician would follow. This procedure is known as Gram staining. First, a Petri dish containing the culture of isolate from patient B was obtained. Using a sterile swab, the culture of isolate was evenly spread on a Mueller Hinton agar plate and then repeated on a second plate. Dipping forceps in alcohol before each use to sterilize, place the antibiotic tabs in the plate following the diagram. On the bottom of the plate, use a marker to divide the plate into sections along the dotted line in the following figure.
Once the plates have been carefully incubated, use a ruler to measure the diameter of the circle that has appeared around each tab. Record the measurements in a table.
The independent variable is the antibiotic while the dependent variable is diameter of the “killing zone” of the antibiotic.
I. Results
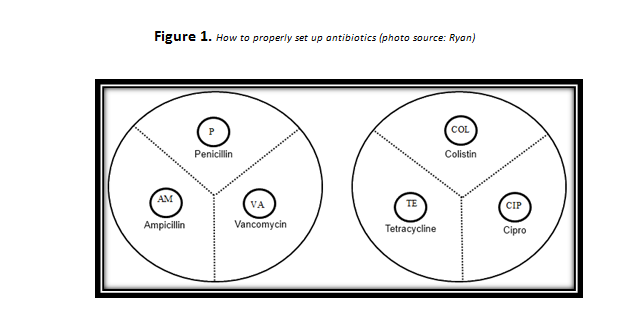
First, Colistin, the only Gram-negative antibiotic, yielded a 1mm killing zone proving that the bacteria were resistant to it. The narrow, Gram-positive antibiotics, Penicillin and Vancomycin, proved to be more effective that Colistin with killing zones of 30mm and 25mm respectively. The bacteria were sensitive to these antibiotics. The broad antibiotics used were Ampicillin, Cipro and Tetracycline. On average, these broad antibiotics performed on par, if not better than the narrow antibiotics with killing zones of 32mm, 30mm and 25mm respectively. The data collected from this experiment has proven the hypothesis to be correct. See the following figure.
Figure 2. This table shows the killing zones (mm) of each antibiotic. (Note, the data for patient A was recorded from another group.)
|
Type of Antibiotic |
Patient A |
Patient B |
|||
|
Antibiotic |
Killing Zone Diameter (mm) |
Resistant, Sensitive, Intermediate |
Killing Zone Diameter (mm) |
Resistant, Sensitive, Intermediate |
|
|
Ampicillin |
Broad |
21 |
Resistant |
32 |
Sensitive |
|
Cipro |
Broad |
33 |
Sensitive |
30 |
Sensitive |
|
Colistin |
Narrow, Gram-negative |
0 |
Resistant |
1 |
Resistant |
|
Penicillin |
Narrow, Gram-positive |
15 |
Resistant |
30 |
Sensitive |
|
Tetracycline |
Broad |
27 |
Sensitive |
25 |
Sensitive |
|
Vancomycin |
Narrow, Gram-positive |
21 |
Sensitive |
25 |
Sensitive |
II. Discussion
The purpose of this study was to put you in the mindset of a physician to determine the appropriate antibiotic for the patient. The hypothesis was: “Broad antibiotics will have “killing zones” with larger diameters than the narrow antibiotics will. Also, narrow, Gram-positive antibiotics will have larger killing zone diameters than narrow, Gram-negative antibiotics.” Based on the data in the above table (and mentioned in the previous section), the hypothesis was accepted.
Since overuse of antibiotics is the leading cause of antibiotic resistance, the selection must be made with thought. This experiment is an appropriate method to determine which antibiotic is best. In patient B, it can be concluded that the bacterial infection is Gram-positive. This is determined because the Gram-negative antibiotic was resisted while the Gram-positive and broad antibiotics were effective. As mentioned before, broad antibiotics should be avoided if a narrow antibiotic could be used. The choices at this point were Penicillin and Vancomycin. Vancomycin was chosen because it is not too strong and is a good starter antibiotic.
This was an important experiment because it gives you an insight to the importance of antibiotics in the medical field. Careful experimentation must be used to determine what type of bacteria the infection is. The importance of this is because physicians need to understand how bacteria are different and how they respond to antibiotics. By understanding the principles of bacteria and antibiotics physicians can then learn how to make sure infection related deaths are lowered and antibiotic resistance is minimized.
V. Cited References
Pinou, Theodora. “Biology 104: General Biology II.” Western Connecticut State University, 2013. February 2013.
Pollack, Andrew. “A Rising Hospital Threat.” The New York Times. The New York Times, 27 Feb. 2010. Web. 21 Feb. 2013.
Ryan, Tyler. Figure 1. Digital image. N.p., 21 Feb. 2013. Web. 10 Mar. 2013.
Solomon, Eldra P., Linda R. Berg, and Diana W. Martin. Biology. 9th ed. Vol. 1. N.p.: Brooks/Cole, 2011. Print.